Another Vaping Hazard: Less-Healthy Mouths
Your lungs might not be your only concern if you're trying electronic cigarettes -- your mouth may pay the price, too.
Your lungs might not be your only concern if you're trying electronic cigarettes -- your mouth may pay the price, too.
Vaping alters the natural bacteria found in the mouth, leaving you more vulnerable to oral infections and inflammation, a new study reports.
The researchers said this study is the first to show that vaping can alter the natural balance of beneficial bacteria (microbiome) in the mouth, adding to the list of potential health effects associated with e-cigarette use.
"Cells that are exposed to e-cigarettes are more susceptible to infections," said the study's senior author, Deepak Saxena. He's a professor of basic science and craniofacial biology at NYU College of Dentistry in New York City.
Saxena said that e-cigarettes also lead to increased inflammation, which harms oral health. And once someone develops inflammation, it's possible to develop white patches in the mouth called leukoplakia that sometimes develop into cancer. However, this study doesn't have enough long-term evidence to show whether or not these changes could lead to oral cancers in the future,
How to Avoid Stained Teeth When You Enjoy Red Wine
You don't have to wind up with stained teeth if you toast the holidays with red wine, an experts say.
You don't have to wind up with stained teeth if you toast the holidays with red wine, an expert says.
"The strength of your enamel and how prone you are to plaque buildup is key to how much your teeth might stain," said Dr. Uchenna Akosa, head of Rutgers Health University Dental Associates, the faculty practice of Rutgers School of Dental Medicine in New Brunswick, N.J.
Akosa called red wine a "triple threat" to a sparkling smile.
"When you drink red wine, you're encountering a triple threat to your teeth's whiteness: anthocyanins, which are the pigments in grapes that give red wine its rich color; tannins, which help bind the pigment to your teeth; and the acidity found in wine, which etches your enamel, making it more porous and it easier for the stain to stick," she said in a Rutgers news release.
Brush Your Teeth To Protect The Heart
Brushing teeth frequently is linked with lower risks of atrial fibrillation and heart failure, according to a new study.
Previous research suggests that poor oral hygiene leads to bacteria in the blood, causing inflammation in the body. Inflammation increases the risks of atrial fibrillation (irregular heartbeat) and heart failure (the heart's ability to pump blood or relax and fill with blood is impaired). This study examined the connection between oral hygiene and occurrence of these two conditions.
The retrospective cohort study enrolled 161,286 participants of the Korean National Health Insurance System aged 40 to 79 with no history of atrial fibrillation or heart failure. Participants underwent a routine medical examination between 2003 and 2004. Information was collected on height, weight, laboratory tests, illnesses, lifestyle, oral health, and oral hygiene behaviours.
During a median follow-up of 10.5 years, 4,911 (3.0%) participants developed atrial fibrillation and 7,971 (4.9%) developed heart failure.
Tooth brushing three or more times a day was associated with a 10% lower risk of atrial fibrillation and a 12% lower risk of heart failure during 10.5-year follow up. The findings were independent of a number of factors including age, sex, socioeconomic status, regular exercise, alcohol consumption, body mass index, and comorbidities such as hypertension.
While the study did not investigate mechanisms, one possibility is that frequent tooth brushing reduces bacteria in the subgingival biofilm (bacteria living in the pocket between the teeth and gums), thereby preventing translocation to the bloodstream.
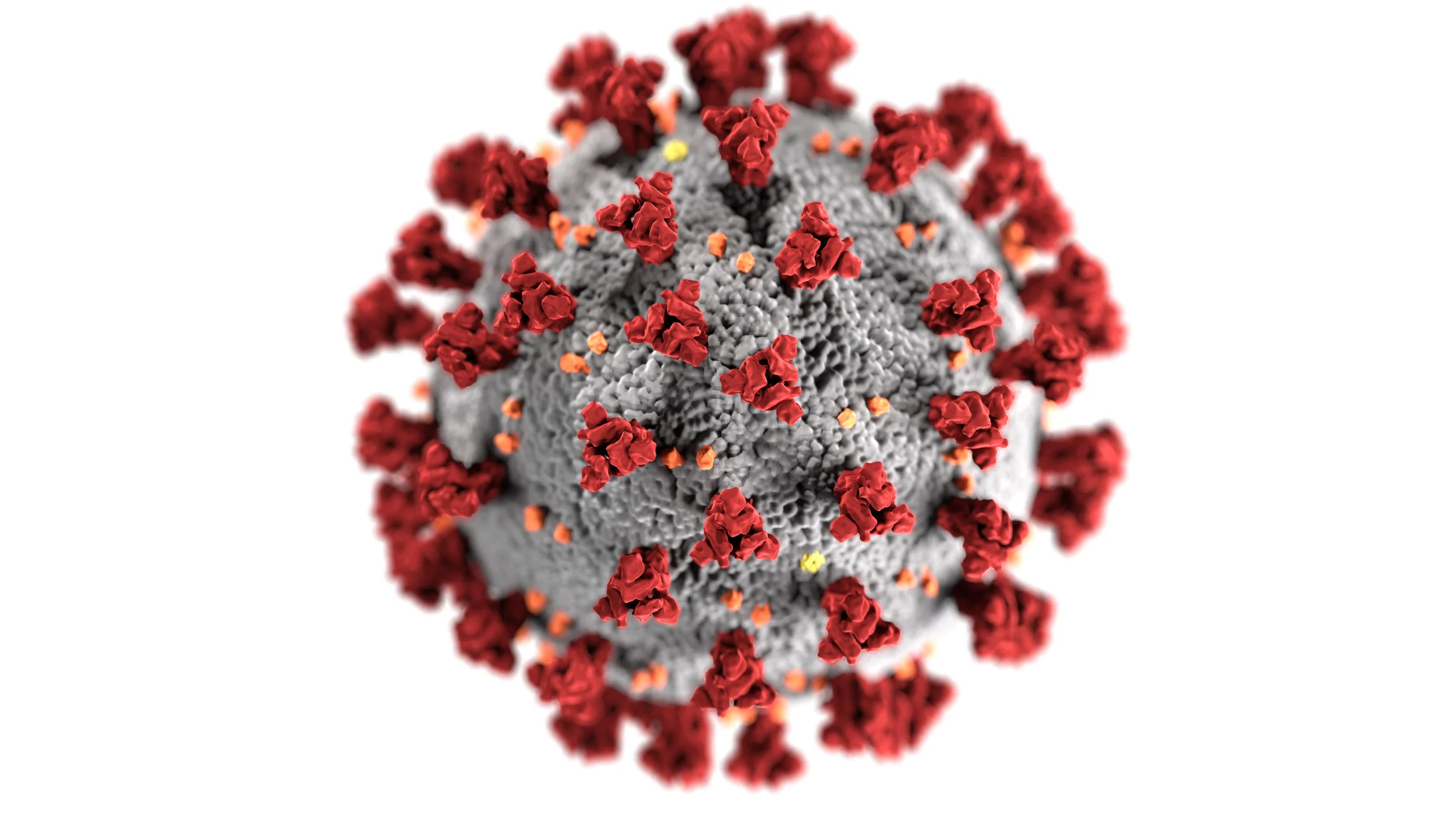
Dentists Already Are Prepared for the Coronavirus
The COVID-19 seems to be in the news daily and has been discussed by people everywhere. But, and this is a good but, the world of dentistry is very prepared for this treat.
It seems like every few years, a new coronavirus pops up and causes some media attention. Such was the case with the 2002 Severe Acute Respiratory Syndrome (SARS) Coronavirus and the 2012 Middle East Respiratory Syndrome (MERS) Coronavirus.
According to the Centers for Disease Control and Prevention (CDC), coronaviruses usually come from animal sources such as bats and camels. Sometimes these coronaviruses cross from animals to humans, such as the previously mentioned SARS and MERS viruses, as well as the new 2019 Novel Coronavirus (COVID-19). The COVID-19 seems to be in the news daily and has been discussed by people everywhere. But, and this is a good but, the world of dentistry is very prepared for this treat.
The CDC notes that the dental community has been doing a very good job of protecting our patients via state-of-the-art infection control practices. The use of personal protective equipment (PPE) including masks, gloves, protective eyewear, and gowns has led to better protection for our staff and patients. Our use of disinfectants, up-to-date sterilization practices, dedicated hand washing, and one-time-use disposable materials also have all helped facilitate safe dental visits for our patients. All of these practices have been the backbone of the CDC’s Standard Precautions.
Special sensory cells in gums protect against periodontitis
Periodontitis is a serious gum disorder induced by an imbalance in the bacteria and other microorganisms of the mouth (the oral microbiome). It is the sixth-most prevalent infectious disease and the most common cause of tooth loss worldwide.
Monell Center Director and President Robert Margolskee, MD, PhD and cell biologist Marco Tizzano, PhD, along with colleagues from Sichuan University, found that the newly identified cells, known as solitary chemosensory cells (SCCs), are present in the gums of mice. Here they express several types of taste receptors along with a downstream coupling protein called gustducin. SCCs are taste-like chemical detectors that sense irritants and bacteria, and biologists have found them throughout the gut, urinary tract, nasal cavities, and now in the gums.
"These sensory cells may provide a new approach for personalized treatment of periodontitis by harnessing a person's own innate immune system to regulate their oral microbiome," said Margolskee.
The team showed that knocking out taste-signaling molecules like gustducin or genetically removing gum SCCs in the mice leads to overgrowth of pathogenic oral bacteria and periodontitis. Conversely, stimulating bitter taste receptors in SCCs promotes the production of anti-microbial molecules.
Mice without gustducin in their SSCs have a more damaging set of microbes living in their mouths compared to normal mice, implying that the lack of gustducin disconnects the sentinel cells' molecular signal to other systems. Importantly, differences in the oral bacterial composition of the gustducin-less mice compared to normal mice occurred before any loss of bone in the gums, implying that differences in the oral microbiome could be used as a harbinger of disease.
Soft drinks found to be the crucial link between obesity and tooth wear
A new study published today in the journal Clinical Oral Investigations, has found that sugar-sweetened acidic drinks, such as soft drinks, is the common factor between obesity and tooth wear among adults.
Scientists from King's College London found that being overweight or obese was undoubtedly associated with having tooth wear. Significantly, they also found that the increased consumption of sugary soft drinks may be a leading cause of the erosion of tooth enamel and dentine in obese patients.
Drawing on data from the National Health and Nutrition Examination Survey 2003-2004, they analysed a representative sample of survey participants of 3,541 patients in the United States. Patient BMI and the level of tooth wear were the exposure and outcome measurements in the analysis. The intake of sugar-sweetened acidic drinks was recorded through two non-consecutive 24-hour recall interviews where the patients were asked to provide details of diet intake across these two days.
"It is the acidic nature of some drinks such as carbonated drinks and acidic fruit juices that leads to tooth wear," said lead author Dr Saoirse O'Toole from King's College London.
Tooth wear is ranked as the third most important dental condition, after cavities and gum disease and the consumption of acidic food and drink is a leading cause of this. Obese patients also have other risk factors such as increased likelihood of gastric reflux disease (heartburn) which was controlled for in this study.
Temporomandibular Joint Dysfunction Symptoms Following Massage Therapy
Researchers have estimated that 65%–85% of Americans experience some symptoms of temporomandibular joint dysfunction (TMD) during their lives. This is perhaps owing to the fact that the temporomandibular joint (TMJ) is the most frequently used joint in the body, moving 2000–3000 times a day. TMD is a condition that encompasses several pathologies of the jaw and the muscles of mastication (chewing). Symptoms of TMD are most common in people between 15 and 45 years of age, and are more common in women than men by a ratio of 5:1. A triad of predisposition, tissue alteration (neuromuscular, skeletal, and dental), and stress sufficient to cause jaw clenching and/or bruxism is usually necessary to provoke TMD.
Symptoms of TMD vary from case to case, but common complaints include: spasm and/or pain in the head, jaw, neck, and shoulder muscles; headaches; earaches; jaw clicking or deviation; limited jaw opening; clenching or grinding of the teeth; and dizziness. Causes can include whiplash, bruxism, malocclusion, anxiety, stress, trigger points, and postural dysfunction.
It is important for patients to seek treatment because muscle contractures may develop and degeneration of the disc, condylar head and articular eminence may occur if not corrected. There are several approaches to the treatment of TMD. These treatment strategies are as diverse as the patients presenting the symptoms. Because each patient presents differently, he or she should be assessed and treated according to his or her distinct needs. Because most of the causes and conditions associated with TMD are irremediable, it has been suggested that treatment be aimed toward symptomatic relief and not cures. Common treatment options include: splint therapy, occlusal adjustment, analgesic medications, surgery, acupuncture, trigger point injections, hydrotherapy, therapeutic ultrasound, electromyopathy, hypnorelaxation, cognitive-behavioral therapy, massage therapy, stress management, and biofeedback. Home care practices such as a soft food diet, a local application of ice, self-massage, hot showers, and stretching have also been suggested as being beneficial.
Treatments that are discussed in the dentistry literature focus on surgical repair, splint therapy, and medication. In addition, some dentists may choose to refer their patients to massage therapists to assist in treatment of this condition. Although support for the use of massage therapy as a part of a comprehensive treatment solution for TMD has been discussed, literature that addresses the effectiveness of massage therapy on TMD is limited and studies report varying degrees of success.
Advancements in Oral Cancer Therapy: The Role of Botanical Compounds in Tumor Management
A plant-based drug called APG-157 has shown signs of helping patients fight oral and oropharyngeal cancers, according to a phase I clinical trial led by the University of California at Los Angeles Jonsson Comprehensive Cancer Center.
The landscape of oral and oropharyngeal cancer treatment is evolving, with new research highlighting the potential of botanical drug candidates to complement traditional oncology protocols. A recent Phase I clinical trial led by the UCLA Jonsson Comprehensive Cancer Center has revealed promising data regarding APG-157, a plant-based drug that targets the inflammatory and microbial environment of oral tumors.
At CJ Henley, DMD, our involvement in the Baptist MD Anderson Head and Neck Tumor Board allows us to integrate these emerging clinical insights into our specialized care for patients navigating cancer treatment.
The Science Behind APG-157: Curcumin and Inflammation
APG-157 is a botanical drug composed of multiple plant-derived compounds, most notably curcumin. The clinical trial demonstrated that when taken orally, high concentrations of curcumin and its metabolic byproducts are absorbed by tumor tissues in as little as three hours.
The significance of this absorption lies in its effect on cytokines—the proteins responsible for driving inflammation within the body. By reducing cytokine concentrations in the saliva, APG-157 may help modulate the inflammatory "microenvironment" that allows tumors to thrive.
Microbiome Modulation and Gram-Negative Bacteria
Beyond inflammation, this therapy addresses the oral microbiome. Researchers found that APG-157 reduced the relative abundance of Bacteroides species, a group of gram-negative bacteria.
Gram-negative bacteria possess a protective outer layer that effectively "hides" them from the immune system. In the context of oral health, an overabundance of these bacteria is closely correlated with the development and progression of oral cancers. Reducing these bacterial populations is a critical step in restoring a healthy oral environment during and after cancer therapy.
A Medically-Informed Approach to Oncology Dental Care
As a practice focused on Complex & Medically Involved Care, we understand that oral cancer treatment requires more than routine dentistry. It requires a deep understanding of how systemic therapies and the oral microbiome interact.
We prioritize a two-hour comprehensive evaluation for our oncology patients to discuss these emerging therapies, manage side effects like xerostomia, and coordinate care with your medical team to ensure the best possible long-term outcomes.
Reviewed and Updated February 2026
Milk from teeth
Dental epithelial stem cells are able to generate all epithelial cell types of the teeth; however, it was not yet clear whether these cells could also produce non-dental cell populations. In a recent paper published in the open access journal Cells, a team of researchers led by Thimios Mitsiadis, professor at the Institute of Oral Biology of the University of Zurich (UZH), has shown for the first time that epithelial stem cells isolated from the continuously growing incisors of young mice are indeed able to form mammary glands in female mice.
In a first set of experiments, after removing all cells of mammary origin, dental epithelial stem cells and mammary epithelial cells were directly injected into the areas where the mammary glands normally develop. The researchers used advanced genetic, molecular and imaging tools that allow the precise follow-up of the transplanted dental stem cells in the mammary gland fat pad of the animals. "The results show that the dental stem cells contribute to mammary gland regeneration, and are able to generate all mammary cell populations and, even more strikingly, milk-producing cells," says Mitsiadis.
This work demonstrates the exceptional plasticity of dental epithelial stem cells to generate not only dental tissues but also other tissues of the body. "These findings represent a major contribution to the understanding of the cellular and molecular mechanisms involved in the regenerative capacity of dental stem cells, and, furthermore, indicate the clinical potential of these specific stem cell populations," Mitsiadis adds.
An Oral Splint that can Reduce Tourette Syndrome Tics
While there is no cure for Tourette syndrome, there are several available options to treat severe tics. These include behavioral (e.g. psychotherapy and cognitive behavioral therapy), pharmacological (e.g. medications that block dopamine in the brain), and more intrusive surgical interventions (e.g. deep brain stimulation, whereby motor areas of the brain receive electrical stimulation). However, the efficacy of these treatments can vary, and patients still frequently suffer from physical, mental, and social disabilities. As an alternative treatment option, researchers at Osaka University have developed a custom-made oral splint. These are typically used for unconscious teeth clenching and grinding, and for temporomandibular disorders such as misalignment of the teeth or jaw. The oral splint is applied to the molars to increase the occlusal vertical dimension, which essentially means that the alignment of the nose, lips, and chin is altered. The study was recently published in Movement Disorders.