BLOG: A PLACE TO FIND THE MOST UP-TO-DATE INFORMATION ABOUT DENTISTRY IN JACKSONVILLE
Evidence grows for vaping's role in gum disease
New studies highlight how e-cigarettes alter oral health and may be contributing to gum disease. The latest research finds that e-cigarette users have a unique oral microbiome that is less healthy than nonsmokers but potentially healthier than cigarette smokers, and measures worsening gum disease over time.
A series of new studies by researchers at NYU College of Dentistry highlights how e-cigarettes alter oral health and may be contributing to gum disease. The latest, published in mBio, finds that e-cigarette users have a unique oral microbiome -- the community of bacteria and other microorganisms -- that is less healthy than nonsmokers but potentially healthier than cigarette smokers, and measures worsening gum disease over time.
"To our knowledge, this is the first longitudinal study of oral health and e-cigarette use. We are now beginning to understand how e-cigarettes and the chemicals they contain are changing the oral microbiome and disrupting the balance of bacteria," said Deepak Saxena, who led the research with Xin Li; both are professors of molecular pathobiology at NYU College of Dentistry.
Gum disease affects nearly half of U.S. adults over 30 years of age. Smoking cigarettes is a known risk factor for developing gum disease, but less is known about the impact of e-cigarettes -- which vaporize nicotine and other chemicals -- on oral health, especially the long-term consequences of vaping.
The researchers studied the oral health of 84 adults from three groups: cigarette smokers, e-cigarette users, and people who have never smoked. Gum disease was assessed through two dental exams six months apart, during which plaque samples were taken to analyze the bacteria present.
Changes to gum health
All participants had some gum disease at the start of the study, with cigarette smokers having the most severe disease, followed by e-cigarette users. After six months, the researchers observed that gum disease had worsened in some participants in each group, including several e-cigarette users.
A key indicator of gum disease is clinical attachment loss, measured by gum ligament and tissue separating from a tooth's surface, leading the gum to recede and form pockets. These pockets are breeding grounds for bacteria and can lead to more severe gum disease. In a study of the same participants published in Frontiers in Oral Health, the research team found that clinical attachment loss was significantly worse only in the e-cigarette smokers -- not non-smokers and cigarette smokers -- after six months.
A unique microbiome
The researchers then analyzed the bacteria found in the plaque samples and determined that e-cigarette users have a different oral microbiome from smokers and nonsmokers -- building on findings the team previously reported in iScience and Molecular Oral Microbiology.
While all groups shared roughly a fifth of the types of bacteria, the bacterial makeup for e-cigarette users had strikingly more in common with cigarette smokers than nonsmokers. Several types of bacteria, including Selenomonas, Leptotrichia, and Saccharibacteria, were abundant in both smokers and vapers compared to nonsmokers. Several other bacteria -- including Fusobacterium and Bacteroidales, which are known to be associated with gum disease -- were particularly dominant in the mouths of e-cigarette users.
When plaque samples were gathered and analyzed in the six-month follow-up, the researchers found greater diversity in bacteria for all groups studied, yet each group maintained its own distinct microbiome.
"Vaping appears to be driving unique patterns in bacteria and influencing the growth of some bacteria in a manner akin to cigarette smoking, but with its own profile and risks to oral health," said Fangxi Xu, a junior research scientist in Saxena's lab and the study's co-first author.
An altered immune response
The researchers found that the distinct microbiome in e-cigarette users was correlated with clinical measures of gum disease and changes to the host immune environment. In particular, vaping was associated with different levels of cytokines -- proteins that help regulate the immune system. Certain cytokines are linked to an imbalance in oral bacteria and can worsen gum disease by making people prone to inflammation and infection.
TNFα, a cytokine that causes inflammation, was significantly elevated among e-cigarette users. In contrast, cytokines IL-4 and IL-1β were lower among e-cigarette users; IL-4 tends to be reduced in people with gum disease and increases after treatment, which suggests that certain bacteria in the mouths of e-cigarette users may be actively suppressing immune responses.
The researchers concluded that the distinct oral microbiome of e-cigarette users elicits altered immune responses, which along with clinical markers for gum disease illustrate how vaping presents its own challenge to oral health.
"E-cigarette use is a relatively new human habit," said Scott Thomas, an assistant research scientist in Saxena's lab and the study's co-first author. "Unlike smoking, which has been studied extensively for decades, we know little about the health consequences of e-cigarette use and are just starting to understand how the unique microbiome promoted by vaping impacts oral health and disease."
This research was supported by the National Institute of Dental & Craniofacial Research (DE025992, DE027074), the National Cancer Institute (CA206105), and the NYU Mega-Grants Initiative. The study included additional collaborators from NYU College of Dentistry, NYU Grossman School of Medicine, and the University of Pennsylvania.
April is Oral Cancer Awareness Month
Every hour, 24-hours-a-day, 365-days-a-year, someone dies of oral or oropharyngeal cancer (cancer of the mouth and upper throat). Yet, if oral cancer is detected and treated early, treatment-related health problems are reduced and survival rates may increase.
Every hour, 24-hours-a-day, 365-days-a-year, someone dies of oral or oropharyngeal cancer (cancer of the mouth and upper throat). Yet, if oral cancer is detected and treated early, treatment-related health problems are reduced and survival rates may increase.
This year an estimated 54,0001 new cases of oral cancer will be diagnosed. Of those individuals, 43 percent will not survive longer than five years, and many who do survive to suffer long-term problems, such as severe facial disfigurement or difficulties with eating and speaking. The death rate associated with oral and oropharyngeal cancers remains particularly high because the cancers routinely are discovered late in their development.
This April, as the nation observes the 22nd Annual Oral Cancer Awareness Month, the Academy of General Dentistry Foundation (agd.org/agd-foundation), the American Academy of Oral and Maxillofacial Pathology (aaomp.org), American Academy of Oral and Maxillofacial Radiology (www.aaomr.org), the American Association of Oral and Maxillofacial Surgeons (myoms.org), the American Academy of Oral Medicine (aaom.com), the American Academy of Periodontology (perio.org), the American College of Prosthodontics (www.prosthodontics.org), the American Dental Hygienists’ Association (www.adha.org), and the California Dental Hygienists’ Association (www.cdha.org) are again joining the non-profit Oral Cancer Foundation in its campaign to raise awareness of oral cancer screenings and the importance of early detection.
Regular oral cancer examinations performed by your oral health professional remain the best method for detecting oral cancer in its early stages.
Be Mindful of Symptoms: Public Urged to “Check Your Mouth”
For the third straight year, the efforts of the Foundation and the dental associations cited above will be bolstered by the Oral Cancer Foundation’s Check Your Mouth™ initiative (www.checkyourmouth.org). Check Your Mouth encourages the public to regularly check for signs and symptoms of oral cancer between dental visits and to see a dental professional if they do not improve or disappear after two or three weeks.
Signs and symptoms of oral cancer which is predominantly caused by tobacco usage and/or excessive alcohol usage may include one or more of the following:
Any sore or ulceration that does not heal within 14 days.
A red, white, or black discoloration of the soft tissues of the mouth.
Any abnormality that bleeds easily when touched (friable).
A lump or hard spot in the tissue, usually border of the tongue (induration).
Tissue raised above that which surrounds it; a growth (exophytic).
A sore under a denture, which even after adjustment of the denture, does not heal.
A lump or thickening that develops in the mouth.
A painless, firm, fixated lump felt on the outside of the neck, which has been there for at least two weeks.
All the above symptoms have the commonality of being persistent and not resolving.
Signs and symptoms of HPV-caused oropharyngeal cancer may include one or more of the following (which may persist longer than two-three weeks):
Hoarseness or sore throat that does not resolve within a few weeks.
A swollen tonsil on just one side. This is usually painless.
A painless, firm, fixated lump felt on the outside of the neck, which has been there for at least two weeks.
A persistent cough that does not resolve after many days.
Difficulty swallowing; a sensation that food is getting caught in your throat.
An earache on one side (unilateral) persists for more than a few days.
All the above symptoms have the commonality of being persistent and not resolving.
Always call your dentist right away if there are any immediate concerns.
Risk Factors
Research has identified a number of factors that may contribute to the development of oral and oropharyngeal cancers. Historically, those at an especially high risk of developing oral cancer have been heavy drinkers and smokers older than age 50, but today the cancer also is occurring more frequently in nonsmoking people due to HPV16, the virus most commonly associated with cervical cancer.
The sexually transmitted human papillomavirus 16 (HPV) is related to the increasing incidence of oropharyngeal cancer (most commonly involving lymphoid tissue occurring in the tonsils or the base of the tongue). Approximately 99 percent of people who develop an HPV oral infection will clear the virus on their own. In approximately 1 percent of individuals, the immune system will not clear the virus and it can lay dormant for decades before potentially causing a cancer, this occurs mostly in a non-smoking population composed of males four to one over females.
If you have never had an oral cancer examination, there is no better time to schedule one than during Oral Cancer Awareness Month in April. When you do, be sure to ask that this examination be made a routine part of all of your future dental check-ups. For a list of local dental professionals who are participating in this year’s event by offering free oral cancer screenings, visit the Oral Cancer Foundation’s website.
For more information about oral cancer and its diagnosis and treatment, visit the websites of the organizations listed below.
About Oral Cancer Awareness Month
Each April, several of the nation’s top dental associations join together with the Oral Cancer Foundation to raise awareness for oral and oropharyngeal cancers. Many dental professionals around the country open their offices to do free screenings to the public during this month each year as well. This is an important reminder to the public that when these cancers are detected and treated early, mortality and treatment related health problems are reduced. For more information visit the Oral Cancer Foundation website at www.oralcancer.org.
Is there a connection between oral health and COVID-19?
Doctors and researchers are investigating the many effects of COVID-19 and its possible impact on the teeth, gums, and oral cavity.
Doctors and researchers are investigating the many effects of COVID-19 and its possible impact on the teeth, gums, and oral cavity.
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) causes the new coronavirus disease 2019 (COVID-19).
This article will discuss the possible links between COVID-19 and oral health.
Is there a link?
There does not appear to be much research suggesting that COVID-19 can lead to poor oral health.
However, one 2021 study suggests that poor oral health can play a part in contracting SARS-CoV-2.
The study notes that the mouth can act as an entry point for SARS-CoV-2 because cells in the tongue, gums, and teeth have angiotensin-converting enzyme-2 (ACE2). This is the protein receptor that allows the virus to enter cells.
In those with poor oral health, the presence of ACE2 receptors appears to be higher.
Another article notes that there may be a connection between gum disease and changes in dental plaque with an increased risk of complications from COVID-19.
The researchers suggest that a lack of oral hygiene can increase the chance of bacteria traveling from the mouth to the lungs. This may then increase the risk of developing a bacterial infection in addition to COVID-19.
COVID-19 and access to oral healthcare
According to the Centers for Disease Control and Prevention (CDC)Trusted Source, oral health is an important part of a person’s overall health and well-being.
Access to dental care is important in reducing the early stages of oral disease.
The COVID-19 pandemic led to reduced opening hours and the closure of dental practices, except in the case of emergency procedures. This has limited people’s ability to access routine care.
The CDC also notes that this lack of access to dental care disproportionately affects those who are from low income households and who rely on dental benefits under Medicaid.
Only 20% of dentists accept Medicaid. Additionally, people who rely on Medicaid dental benefits have experienced restrictions and reductions in their coverage.
COVID-19 and gingivitis
Gingivitis refers to inflammation of the gums.
Some symptoms of gingivitis include:
red, swollen gums
bleeding gums when brushing or flossing
bad breath
an unpleasant taste in the mouth
Poor oral hygiene can lead to the accumulation of bacteria that stick to the teeth and form dental plaque. This is a common cause of gingivitis.
The authors of one 2021 case report speculate that having a debilitating disease such as COVID-19 may mean that a person is less likely to practice good oral hygiene. This enables dental plaque to grow, which increases the risk of gingivitis.
The researchers also suggest that bleeding gums may be a symptom of COVID-19. They observed that symptoms of gingivitis reduced after COVID-19 subsided.
However, these findings are based on a study of three people. More research in a wider population is necessary to confirm them.
Can COVID-19 cause tooth sensitivity?
There does not appear to be any research suggesting that there is a direct link between COVID-19 and tooth sensitivity.
A person experiences tooth sensitivity when the enamel, which is the hard outer layer that protects the teeth, becomes damaged or weakened.
Some symptoms of tooth sensitivity include:
pain or discomfort while chewing
sensitivity to hot or cold foods
pain after exposure to cold air
sensitivity to sweet or acidic foods and drinks
For mild cases of tooth sensitivity, a person can use desensitizing toothpaste. They can also try using extra soft toothbrushes.
If the symptoms persist, a person may wish to consult a dentist.
COVID-19 and dry mouth
Dry mouth, or xerostomia, occurs when there is inadequate saliva to keep the mouth moist. This makes it difficult to break down food, wash food particles away from the mouth, and swallow food.
Dry mouth may be an early symptom of COVID-19, and it was one of the most common oral symptoms reported by 108 people in a study in The Lancet. However, the reasons for this are still unclear.
The study authors say that dry mouth may be a direct effect of the SARS-CoV-2 virus infecting and damaging the salivary glands. It may also occur due to poor oral hygiene or as a side effect of COVID-19 treatment.
Without treatment, dry mouth can increase the riskTrusted Source of tooth decay and infection in the mouth.
COVID-19 and oral ulcers
Like other viral infections, SARS-CoV-2 impairs the immune system and makes a person susceptible to other secondary conditions.
Some peopleTrusted Source recovering from this infection have observed ulcers in their mouth. For some, doctors have found these ulcers to be thrush-like, while others have seemed fairly unspecific.
An ulcer may develop as a white patch on the tongue, gums, or roof of the mouth.
Some other symptoms include:
white or red bumps in the mouth
dull pain
discomfort while eating and drinking
a burning sensation
According to the National Health Service (NHS), mouth ulcers tend to resolve on their own in 1–2 weeks. A person should consult a doctor if ulcers persist for longer than 3 weeks, as this could indicate another opportunistic infection.
Alternatively, a local pharmacist can recommend some simple measures to treat an ulcer a home. These measures could take the form of an antimicrobial mouthwash, a topical gel or cream, medicated lozenges, or a mouth spray.
Can COVID-19 cause cracked teeth?
According to the American Dental Association, dentists have noted a 59% increase in teeth grinding, or bruxism, and a 53% increase in chipped and cracked teeth since the start of the COVID-19 pandemic.
They suggest that this can occur as a result of higher anxiety levels during the pandemic and poor posture resulting from a work-from-home environment.
The dentists explain that anxiety and poor posture can cause people to clench their jaw and grind their teeth. These are involuntary behaviors that stem from added stress. The result is increased pressure on the teeth that weakens them and makes them more prone to crack.
Cases of chipped or cracked teeth have also occurred in people with severe COVID-19. One studyTrusted Source suggests that people in critical care, such as those who need ventilators, experience a range of complications, including chipped teeth.
Summary
Amid the rise in oral diseases during the pandemic, researchers are trying to determine whether they are due to COVID-19 or secondary factors such as stress, poor posture, or other conditions.
Although there is no concrete evidence yet to definitively link COVID-19 to oral health, people should try to practice good personal and oral hygiene as a form of disease prevention.
What is bruxism or teeth grinding?
Bruxism is when a person grinds or clenches their teeth while not chewing. It usually occurs during sleep, but it can also happen during waking hours. Often, a person is not consciously aware that they are doing it.
Teeth grinding involves making a chewing motion in which the teeth rub against each other. Clenching is when a person holds their teeth together and clenches the muscles without moving the teeth back and forth.
People can grind or clench their teeth during the day or night. According to the United Kingdom’s Bruxism Association, 8–10% of the population experience it.
In this article, we look at the signs, diagnosis, and treatment of bruxism. We also explain the differences between bruxism during sleep and when awake.
Signs of sleep bruxism
Sleep bruxism is a type of sleep disorder. The symptoms of sleep bruxism that people may notice when awake include:
facial pain
jaw pain and stiffness
clicking, popping, or grinding noises when moving the jaw
a dull headache
sensitive, loose, or broken teeth
worn teeth
broken or loose fillings
People can also experience ear pain because the temporomandibular joint (TMJ) — the joint that allows the jaw to open and shut — is very close to the ear. People may also have referred pain, which is when someone feels pain in a location other than its source.
Although people with bruxism during sleep often cannot feel that they are clenching or grinding the teeth, people who sleep near them may be able to hear the noise it causes.
Awake bruxism
Awake bruxism is different than sleep bruxism, as it is not a sleep disorder. Instead, it is an unconscious habit.
Often, awake bruxism does not cause teeth grinding. Instead, people are more likely to clench their teeth or tense the muscles around the jaw. Awake bruxism also causes aching around the jaw, dull headaches, and stiffness. However, in cases where there is no grinding, the condition may not wear the teeth in the same way.
As with sleep bruxism, awake bruxism happens involuntarily. People may notice that they are more prone to it when they are concentrating or feel stressed.
What causes bruxism?
Bruxism does not always have a single or identifiable cause, but a number of factors are associated with it. These factors vary depending on the type of bruxism.
Primary bruxism
Primary bruxism occurs on its own and does not result from another condition. Some of the known factors that contribute to it include:
Growing teeth: Bruxism is common in young children, with up to 40%Trusted Source experiencing it, usually when their teeth are growing. However, because the teeth and jaw grow quickly during childhood, the bruxism usually resolves on its own without causing lasting damage.
Misaligned bite: In some people, bruxism may happen because either a person’s bite is not aligned or they have missing teeth. Irritation in the mouth may also contribute to grinding or clenching.
Stress: One of the main causes of bruxism in adults, whether it occurs during sleep or when awake, is stress. A 2020 systematic review found that there was a significant association between stress and bruxism, but more research is necessary to understand the relationship.
Smoking, alcohol, and caffeine: A 2016 review of previous research found that the use of these substances was also associated with bruxism. People who smoked or drank alcohol regularly were about two times more likely to have bruxism, while those who drank more than 8 cups of coffee per day were 1.5 times more likely.
Secondary bruxism
Secondary bruxism occurs as a result of another medical condition or circumstance, such as:
Mental health conditions: Anxiety and depression are associated with bruxism. This association may be due in part to stress, which can contribute to these conditions.
Neurological conditions: Conditions such as Huntington’s disease and Parkinson’s disease can cause movement during sleep, which may result in bruxism.
Medications: Bruxism can be a side effect of certain medications, including some antidepressants and antipsychotics. A 2018 study found a link between selective serotonin reuptake inhibitors (SSRIs) and bruxism. Fluoxetine (Prozac) and sertraline (Zoloft) were the most common culprits out of the studied drugs.
Sleep apnea: Sleep apnea is a condition that causes breathing to stop temporarily during sleep. It can reduce sleep quality and cause frequent arousals, which may be why it is a risk factor for bruxism. By disturbing sleep, sleep apnea may promote teeth grinding or clenching.
What are the long-term effects of bruxism?
Long-term damage from bruxism may cause:
tooth sensitivity, due to enamel wearing away
gum inflammation or bleeding
loose teeth
damage to dental work, such as crowns and fillings
flattened or short teeth
tooth fractures
TMJ syndrome, which causes pain, tension, and difficulty chewing
Diagnosis
A dentist can diagnose bruxism by performing a dental examination. They may notice:
worn tooth enamel
flattened, fractured, or chipped teeth
loose or damaged crowns and fillings
enlarged jaw muscles
Tooth wear can also result from overly vigorous brushing, abrasives in toothpaste, acidic soft drinks, and hard foods, but a trained professional can tell the difference between the characteristic wear patterns of each cause.
Treatment
Various treatments and strategies may help with bruxism. These include:
Mouthguard or mouth splint
A dentist may recommend wearing a mouth splint or mouthguard during sleep to protect the teeth from damage. These devices can help by evening out the pressure across the jaw, providing a physical barrier between the teeth, and reducing the noise of teeth grinding.
Mouthguards for bruxism usually consist of flexible rubber or plastic. A dentist can create one that is tailored to an individual’s teeth, or a person can buy an over-the-counter (OTC) version. OTC versions may be less comfortable.
Mouth splints are typically made of harder plastic and fit directly onto the teeth. Some splints fit over the top teeth, while others fit on the bottom teeth. Depending on the design, a splint will keep the jaw in a more relaxed position or provide a barrier so that the splints, rather than the teeth, sustain any damage.
It is not advisable to use generic mouthguards for sports, as they can be bulky and cause significant discomfort.
Medication
Taking a nonsteroidal anti-inflammatory drug (NSAID), such as ibuprofen, may help relieve any pain and swelling associated with bruxism.
In some cases, a doctor may also recommend the short-term use of a medication to relax the muscles and stop the cycle of teeth grinding. This approach gives the jaw muscles a chance to rest, which may reduce symptoms.
If a medication could be causing bruxism as a side effect, a person may wish to speak with a doctor about changing to an alternative. A person should never stop a medication or change the dosage without consulting a doctor first.
Biofeedback
Biofeedback is a type of therapy that helps someone become aware of involuntary bodily functions, such as breathing or heart rate, and teaches them to control them.
There is not a lot of research on the effectiveness of biofeedback for treating bruxism, but a 2018 review did find some evidence that a specific biofeedback tool known as contingent electrical stimulation improved symptoms after several nights of use.
Botox
In severe cases of bruxism, injections of botulinum toxin, or Botox, can paralyze the muscles responsible for sleep bruxism to stop teeth grinding. However, Botox can be expensive, and regular injections are necessary to maintain the effects.
Treatment for underlying conditions
If a person with bruxism also experiences stress, anxiety, or depression, seeking help for these conditions may help with their teeth grinding.
Usually, treatment for these mental health conditions involves a combination of talk therapy and medication to reduce the symptoms, but as some SSRIs can cause bruxism as a side effect, a person may wish to start with therapy first.
Alternatively, if an individual has a condition such as sleep apnea, speaking with a doctor about this may allow them to get a diagnosis and treatment. For example, some people with sleep apnea benefit from using a continuous positive airway pressure machine to prevent sleep disruptions.
Prevention
People with primary bruxism may be able to reduce or prevent the symptoms by practicing self-care. For example, they can try:
avoiding alcohol, tobacco, and caffeine
refraining from chewing gum, as this may increase wear and tear or encourage more grinding
applying gentle heat to the jaw to relieve pain and tension
reducing avoidable stress and taking steps to manage unavoidable stress
External events and circumstances can cause stress, but it can also come from how people perceive those events. In either case, there are ways to manage it.
Seeking support, making time for relaxation, and practicing mindfulness can help. People may also wish to try breathing exercises, meditation, yoga, or other relaxation techniques.
Frequently asked questions
Here are some answers to questions that people often have about bruxism.
Can bruxism cause tinnitus?
It is possible that bruxism and tinnitus might be linked. According to the American Tinnitus Association, tinnitus can occur if the TMJ becomes damaged. As bruxism directly affects this joint, it may lead to tinnitus.
Is bruxism hereditary?
An older review of previous research concluded that there is some evidence that bruxism may run in families. However, no study has identified specific genes that are related to it, and genetics is likely only one of many contributing factors.
Summary
Bruxism is when a person grinds or clenches their teeth involuntarily. It can occur when someone is awake or asleep, causing facial pain, jaw stiffness, and headaches. In the long term, teeth grinding can damage the teeth, gums, or jaw joint.
A dentist can diagnose bruxism during a dental exam. Treatment focuses on reducing damage to the teeth via a mouthguard or mouth splint and addressing factors that might be contributing to the bruxism. This may involve reducing stress, changing medications, or treating associated conditions, such as sleep apnea.
How does acid reflux affect the tongue?
Acid reflux causes the contents of the stomach to move back up the esophagus, causing a burning sensation in the throat. Persistent acid reflux, or gastroesophageal reflux disease (GERD), may also affect the tongue.
Acid reflux causes the contents of the stomach to move back up the esophagus, causing a burning sensation in the throat. Persistent acid reflux, or gastroesophageal reflux disease (GERD), may also affect the tongue.
Laryngopharyngeal reflux is the medical term for acid that reaches the throat because of reflux. Changes to the tongue are an uncommon symptom.
An isolated 2016 study in India found that out of 142 participants with GERD, 2%Trusted Source had swelling and inflammation of the tongue, while 0.7% had red lesions on the tongue.
In this article, we will look at how acid reflux affects the tongue, including whether it can cause mouth sores, dry mouth, or a white tongue.
Can acid reflux affect the tongue?
It is not common for acid reflux to affect the appearance of the tongue, especially if it is infrequent. However, frequent acid reflux, or GERD, often causes oral symptoms. The medical name for this is laryngopharyngeal reflux, which occurs when acid reaches the throat. Some common examples include:
persistent sore throat
burning in the throat or mouth
bad breath
A less common symptom of GERD is damage to the tongue. This occurs when acid reaching the mouth damages tissues in the mouth over time. It can also erode the teeth. An individual 2016 study from India found that in people with GERD:
44% had dental erosion
25.5% had severe gum disease (periodontitis)
9.9% had mild gum disease
Less common symptoms included red lesions on the gums, roof of the mouth, and tongue. However, as this is a single study, more research is necessary to confirm the results.
Some systems of medicine consider tongue changes to be a method for diagnosing diseases elsewhere in the body. For example, a 2020 case control observational study based on the principles of Traditional Chinese Medicine (TCM) found that people with GERD had more “fur” on certain parts of their tongue than those without the disease.
The researchers stated that this could indicate the presence and severity of GERD, but they also call for larger trials to confirm this, as their study included only 67 participants.
Can acid reflux cause mouth sores?
Yes, it is possible for frequent or severe acid reflux to cause sore patches, or lesions, in the mouth. These can occur on the gums, tongue, or palate.
However, this is an uncommon symptom, and can occur for other reasons. More common conditions that cause mouth sores include canker sores and cold sores.
Can acid reflux cause dry mouth?
There is not much research on the connection between acid reflux and dry mouth. However, a 2018 study suggests that swallowing saliva may help neutralize stomach acid. It is possible that people who do not produce enough saliva may have a more acidic stomach, worsening their reflux.
The study found that treating dry mouth also reduced acid reflux. However, more research would have to find similar conclusions to support this as an effective treatment.
In addition to feeling as though the mouth is dry, signs of a dry mouth include:
excessive thirst
bad breath
dry gums or tongue
Can acid reflux cause a metallic taste in the mouth?
People with acid reflux may experience changes in their sense of taste. A sour or bitter taste is common, but it may also taste metallic to some.
Other changes to taste and smell are also possible. A 2017 study found that many participants with GERD reported they were less sensitive to sweet, salty, and bitter tastes and smells than they were before they developed the illness. The researchers noted an association between these changes and the severity of symptoms.
Can acid reflux cause a white tongue?
Research so far has not shown a strong connection between acid reflux and a white coating on the tongue. A 2020 study drawing on TCM found that people with GERD had more “fur” on certain parts of the tongue, but this did not coat the whole tongue. Additionally, this was a small study, so may not apply to a larger population.
However, there is an association between some drugs that doctors use to treat GERD and yeast overgrowth, which can cause a white tongue. A 2017 review noted that in some studies, people taking drugs known as H2 antagonists had higher rates of Candida albicans (a type of yeast) in their digestive tracts, particularly in the esophagus.
Scientists believe that suppressing stomach acid production may allow species of yeast that typically grow at harmless levels, such as C. albicans, to become opportunistic. Doctors can address this through antifungal drugs as well as measures that protect the microbiome. These measures may include:
taking prebiotics, which are substances that feed beneficial bacteria
taking probiotics, which involves taking live bacterial cultures
getting adequate nutrition
People with suppressed immune systems, such as those receiving chemotherapy or who have HIV or AIDs, are at a higher risk of opportunistic infections such as C. albicans than the rest of the population.
Why do teeth turn black?
Black teeth can be a sign of an underlying decay or cavities, or may be the result of staining. Different foods and drinks can leave behind a bit of pigment, causing the teeth to turn black.
Black teeth can be a sign of an underlying decay or cavities, or may be the result of staining. Different foods and drinks can leave behind a bit of pigment, causing the teeth to turn black.
Teeth owe their color to the high amount of calcium found in the outer layer of the teeth, known as the enamel.
Over time, additional elements left behind by foods and drinks can start to make teeth yellow or gray. However, if the teeth turn black, a person should visit a dentist as soon as possible.
What causes teeth to turn black?
Teeth consist of three layers:
Enamel: This is the hard outer layer of the tooth.
Dentin: Dentin is the layer beneath a tooth’s enamel. It contains microscopic tubes that allow heat, cold, and acid to stimulate nerve endings. Damage to enamel can expose dentin.
Pulp: This is the center of the tooth. The pulp of the tooth contains blood vessels, connective tissue, and nerves.
Teeth will appear black due to discoloration of the enamel. Teeth can turn black from either external or internal causes.
External causes
External causes of teeth turning black come from the outside of the tooth.
These can include:
damage to the enamel
stains
tartar buildup
Some direct causes of staining include:
frequently eating or drinking a dark food product, such as coffee
taking certain medications, such as liquid iron supplements
using certain mouth rinses and toothpastes
using tobacco
having crowns and fillings made with silver sulfide
Internal Causes
The tooth may also appear black when damage occurs from the inside. The most common causes of black teeth in these cases are decay or cavities. For example, a tooth with a pulp infection or a dead tooth may turn black.
The damage starts on the inside and works its way to the surface. The black color of the tooth may first appear in spots and eventually cover the entire tooth if a person does not seek treatment.
Symptoms
It is unusual for a tooth to quickly change from a whitish hue to black. A person will typically notice some other signs before the tooth starts to turn black.
A person’s teeth may become more sensitive, resulting in pain when eating or drinking, before teeth discolor. The teeth may also develop small dots that appear black, often near the gum line. This is a common occurrence in children who have black teeth.
When tartar is the cause, a person will probably notice black coloration on the outside of the molars or the inside of the front teeth. Tartar will continue to build up the stain unless a dentist removes it. In these cases, holes may appear as the enamel erodes.
Preventing stains
People concerned about developing black teeth should be sure to practice proper dental hygiene. This includes:
brushing teeth twice a day with fluoride toothpaste
cleaning between the teeth with floss or interdental cleaners daily
attending regular dentist check ups
People may also benefit from avoiding or reducing their intake of the following:
coffee
cola
black tea
red wine
tobacco products
Treatment
It is not usually possible to get rid of black teeth at home. Home whitening kits may help with mild discoloration, but black teeth typically require professional treatment.
A dentist will examine the teeth to diagnose the underlying cause and determine the right treatment.
What if tartar is the cause?
A dentist will need to remove the buildup when tartar is the cause, typically by scraping the tartar off the teeth. The dentist may need to use ultrasonic instruments that use vibration to break up the tartar and make it easier to remove.
What if decay is the cause?
In cases of decay, it is unlikely that a dentist will be able to improve the black teeth through a simple cleaning. They will instead need to remove the decayed portion of the tooth.
When is removal necessary?
Sometimes a dentist will have to remove black teeth.
If the decay is in one part of the tooth, the dentist might be able to remove the affected portion and close the hole with a filling. If the decay has reached a large section of the tooth, the dentist will remove all the decay and place a crown over the top of the tooth.
However, if the damage to the tooth is too severe to recover with a crown or filling, the dentist may need to remove the entire tooth instead.
Takeaway
A dentist can determine if a tooth has turned black due to staining, tartar buildup, or decay. People will need professional help to treat the black teeth, no matter the cause.
Practicing proper dental hygiene can help Trusted Source prevent black teeth. After having a black tooth removed, a person may never have black teeth again with proper care.
Could Losing Your Wisdom Teeth Enhance Your Sense of Taste?
Having your wisdom teeth yanked could have one culinary up side: Heightening your sense of taste?
So claims a new study that challenges previous research on the issue.
"Prior studies have only pointed to adverse effects on taste after extraction, and it has been generally believed that those effects dissipate over time," said study senior author Richard Doty. He is director of the Smell and Taste Center at the University of Pennsylvania, in Philadelphia.
"This new study shows us that taste function can actually slightly improve between the time patients have surgery and up to 20 years later," Doty said in a Penn Medicine news release. "It's a surprising but fascinating finding that deserves further investigation to better understand why it's enhanced and what it may mean clinically."
For the study, the investigators analyzed data from 1,255 people who were evaluated at the smell and taste center over 20 years. Of those, 891 had undergone wisdom tooth extraction and 364 had not.
The participants were tested on their ability to detect sweet, salty, sour or bitter tastes. For all four tastes, the wisdom tooth extraction group outperformed the control group, according to the study published recently in the journal Chemical Senses.
People who've had wisdom teeth extracted typically have an average 3% to 10% long-term improvement in their ability to taste, the researchers concluded.
There are two possible explanations, the study authors suggested.
Wisdom tooth extraction may damage nerves that control taste buds in the front of the mouth, which releases restrictions on nerves that control taste buds in the back of the mouth, boosting whole-mouth sensitivity.
The second possibility is that nerve damage from wisdom tooth extraction may cause taste hypersensitivity, according to the report.
"Further studies are needed to determine the mechanism or mechanisms behind the extraction-related improvement in taste function," Doty said. "The effects are subtle, but may provide insight into how long-term improvement in neural function can result from altering the environment in which nerves propagate."
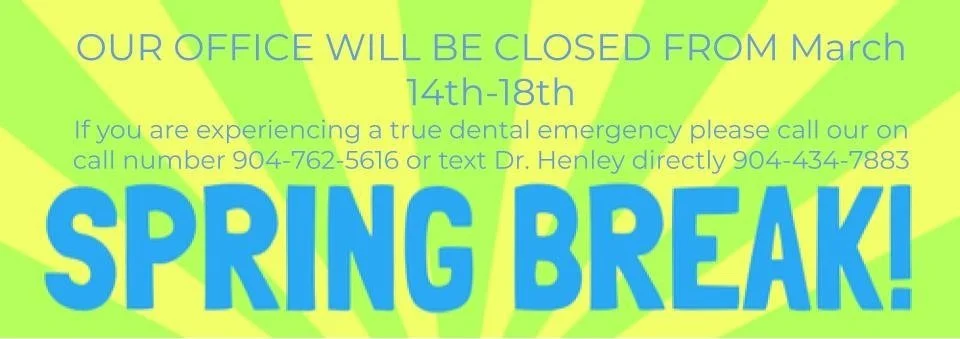
Spring Break
OUR OFFICE WILL BE CLOSED FROM March 14th-18tt. If you are experiencing a true dental emergency please call our on call number 904-762-5616 or text Dr. Henley directly 904-434-7883
OUR OFFICE WILL BE CLOSED FROM March 14th-18th. If you are experiencing a true dental emergency please call our on call number 904-762-5616 or text Dr. Henley directly 904-434-7883
Could a Chewing Gum in Pregnancy Help Prevent Premature Deliveries?
Gum disease has been linked to an increased risk for preterm birth, and now new research suggests that chewing sugar-free gum with xylitol during pregnancy may lower this risk.
The study took place in Malawi, Africa, which has one of the world's highest rates of preterm delivery. Experts are quick to caution that it's too early to say that all pregnant women should start chewing xylitol gum to prevent preterm birth.
Each year, about 15 million babies are born before the 37th week of pregnancy, and this number is on the rise, according to the World Health Organization. Babies who are born too early have more health problems at birth and later in life than those born at full term.
"As a field, we have not been terribly successful in identifying interventions that reduce the risk of preterm birth. And to achieve preterm birth prevention with a simple, fairly cheap intervention in a lower resource setting with one of the highest rates of preterm births worldwide is remarkable," said Dr. Blair Wylie. She is director of maternal-fetal medicine at Beth Israel Deaconess Medical Center in Boston, and was not involved in the study. "This has the potential to save lives in these lower-income settings that bear a disproportionate burden of preterm birth globally."
Xylitol is known to reduce inflammation and improve oral health, explained study author Dr. Kjersti Aagaard. She is a professor in maternal-fetal medicine and vice chairwoman of obstetrics and gynecology at Texas Children's and Baylor College of Medicine in Houston.
"Oral health and the rest of your body health are intimately linked," Aagaard said. "Preterm birth is a challenging problem, and this is a simple intervention based on really good science."
The study took place over 10 years and included more than 10,000 women from eight health centers in Malawi. All of the women were educated about oral health care and other ways to prevent preterm birth. Half of the women were also asked to chew xylitol gum for 10 minutes once or twice a day throughout their pregnancy.
Pregnant women who chewed the gum were less likely to deliver early, compared with women who received education alone — 12.6% versus 16.5%. What's more, fewer babies born to gum-chewing moms weighed 5.5 pounds or less at birth, the study found. Women also saw improvements in their oral health.
"People sometimes think there's nothing we can do about preterm birth, but that's not true," Aagaard said. "We don't have a magic bullet but providing some spread between children, stopping smoking, and treating underlying diseases are all things that can reduce the preterm birth rate, and chewing xylitol gum seems to also make a difference for pregnant women in Malawi."
Studies in the United States have looked at improving dental health during pregnancy with deep-teeth cleaning or scaling and planing to remove plaque and tartar on the teeth and below the gums, but this didn't seem nearly as effective as simply chewing xylitol gum, Aagaard said.
The study was presented Thursday at a virtual meeting of the Society for Maternal-Fetal Medicine. Findings presented at medical meetings should be considered preliminary until published in a peer-reviewed journal.
Experts who were not involved with the study were quick to caution that these results can't be generalized to other groups of women yet, but they noted that the link between poor oral health and preterm birth is well established.
"Xylitol may alter the oral microbiome, leading to healthier gums, less systemic inflammation, and therefore less preterm birth," said Wylie.
But, she added, there are likely key differences in the oral flora and oral habits of women in the study and women in other parts of the world. "It's premature to suggest everyone chew xylitol gum in pregnancy," Wylie said.
Dr. Cynthia Gyamfi-Bannerman, professor and chairwoman of obstetrics, gynecology and reproductive sciences at University of California, San Diego Health Sciences, agreed.
"This particular type of gum has been shown to decrease cavities, and there has always been the suggestion of a relationship between periodontal health and preterm delivery," she said. "Dental health is likely an important part of pregnancy health. Pregnant individuals should continue seeing their dentists and incorporating oral hygiene into health care while pregnant."
The next step, the researchers said, is to conduct similar studies in other parts of the world, including the United States. That would help determine whether the intervention would be helpful in places where there may be lower levels of preterm birth tied to oral health.
Pet dental care
Dental health is a very important part of your pet’s overall health, and dental problems can cause, or be caused by, other health problems. Your pet’s teeth and gums should be checked at least once a year by your veterinarian to check for early signs of a problem and to keep your pet’s mouth healthy.
What is veterinary dentistry, and who should perform it?
Veterinary dentistry includes the cleaning, adjustment, filing, extraction, or repair of your pets' teeth and all other aspects of oral health care. These procedures should be performed by a veterinarian or a board-certified veterinary dentist. Subject to state or provincial regulation, veterinary technicians are allowed to perform certain dental procedures under the supervision of a veterinarian.
The process begins with an oral exam of your pet’s mouth by a veterinarian. Radiographs (x-rays) may be needed to evaluate the health of the jaw and the tooth roots below the gumline. Because most dental disease occurs below the gumline, where you can’t see it, a thorough dental cleaning and evaluation are performed under anesthesia. Dental cleaning includes scaling (to remove dental plaque and tartar) and polishing, similar to the process used on your own teeth during your regular dental cleanings.
Oral health in dogs and cats
Your pet’s teeth should be checked at least once a year by your veterinarian for early signs of a problem and to keep your pet’s mouth healthy.
Have your pet’s teeth checked sooner if you observe any of the following problems:
Bad breath
Broken or loose teeth
Extra teeth or retained baby teeth
Teeth that are discolored or covered in tartar
Abnormal chewing, drooling, or dropping food from the mouth
Reduced appetite or refusal to eat
Pain in or around the mouth
Bleeding from the mouth
Swelling in the areas surrounding the mouth
Some pets become irritable when they have dental problems, and any changes in your pet’s behavior should prompt a visit to your veterinarian. Always be careful when evaluating your pet’s mouth, because a painful animal may bite.
Causes of pet dental problems
Although cavities are less common in pets than in people, they can have many of the same dental problems that people can develop:
Broken teeth and roots
Periodontal disease
Abscesses or infected teeth
Cysts or tumors in the mouth
Malocclusion, or misalignment of the teeth and bite
Broken (fractured) jaw
Palate defects (such as cleft palate)
Periodontal disease is the most common dental condition in dogs and cats – by the time your pet is 3 years old, he or she will very likely have some early evidence of periodontal disease, which will worsen as your pet grows older if effective preventive measures aren’t taken. Early detection and treatment are critical, because advanced periodontal disease can cause severe problems and pain for your pet. Periodontal disease doesn’t just affect your pet’s mouth. Other health problems found in association with periodontal disease include kidney, liver, and heart muscle changes.
It starts with plaque that hardens into tartar. Tartar above the gumline can often easily be seen and removed, but plaque and tartar below the gumline is damaging and sets the stage for infection and damage to the jawbone and the tissues that connect the tooth to the jaw bone. Periodontal disease is graded on a scale of 0 (normal) to 4 (severe).
The treatment of periodontal disease involves a thorough dental cleaning and x-rays may be needed to determine the severity of the disease. Your veterinarian or a board-certified veterinary dentist will make recommendations based on your pet’s overall health and the health of your pet’s teeth, and provide you with options to consider.
Why does dentistry require anesthesia?
When you go to the dentist, you know that what’s being done is meant to help you and keep your mouth healthy. Your dentist uses techniques to minimize pain and discomfort and can ask you how you are feeling, so you accept the procedures and do your best to keep still. Your pet does not understand the benefit of dental procedures, and he or she reacts by moving, trying to escape, or even biting.
Anesthesia makes it possible to perform the dental procedures with less stress and pain for your pet. In addition, anesthesia allows for a better cleaning because your pet is not moving around and risking injury from the dental equipment. If radiographs (x-rays) are needed, your pet needs to be very still in order to get good images, and this is unlikely without heavy sedation or anesthesia.
Although anesthesia will always have risks, it’s safer now than ever and continues to improve so that the risks are very low and are far outweighed by the benefits. Most pets can go home the same day of the procedure, although they might seem a little groggy for the rest of the day.